Occasional heartburn is among the commonest of symptoms. Ask any group of adults if they have had heartburn in the last year, and a third will put up their hands.
There are a number of things you can do to avoid simple heartburn that occurs now and then.
It is important to distinguish simple heartburn from long-standing heartburn that keeps recurring. This could be a sign of an underlying condition such as gastroesophageal reflux disease (GERD).
If the heartburn is frequent, or persistent it’s important to see a doctor so that you receive an accurate diagnosis and the right treatment.
What is Heartburn?
Heartburn is a burning sensation in the chest behind the breastbone. This accounts for the “heart” in heartburn. Other than the name and the location, heartburn is not related to chest pain (angina) due to heart disease. Nevertheless, while chest pain or chest pressure may indicate acid reflux, it is right for anyone with this kind of pain or discomfort to seek urgent medical evaluation. Possible heart conditions must always be excluded first.
“Indigestion” is sometimes used to describe heartburn, but this term is imprecise and people use it to describe anything from diarrhea to belching.
“Dyspepsia” describes pain in the upper abdomen (below the chest) that resembles that of a peptic ulcer. It is important not to confuse dyspepsia with heartburn because the treatments are quite different.
What Causes Heartburn?
In order to assist digestion, the stomach produces a very strong acid called hydrochloric acid. We are normally unaware of this since the stomach is designed to withstand this acid. However, the esophagus or swallowing tube is not so protected. If acid escapes back from the stomach into the esophagus (gastroesophageal reflux), it irritates or damages it.
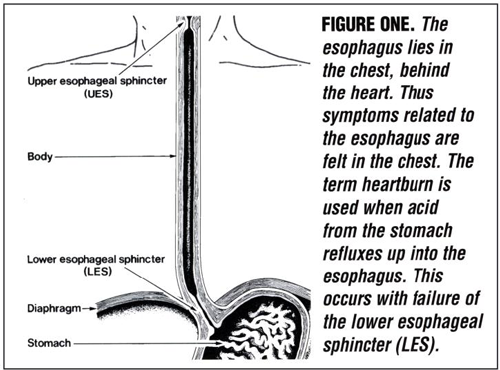
We experience heartburn when reflux – the back-flow of stomach contents – occurs. To prevent this reflux, the lower esophageal sphincter (LES), a band of muscles at the lower end of the esophagus acts like a gate or valve. It permits food to pass down, and then closes to prevent gastric contents from coming back up (Figure One).
This works well most of the time, but many things such as overeating, obesity, aging, and some medicines may compromise this protective mechanism. Hiatus hernia (protrusion of part of the stomach from the abdomen into the chest) can also compromise LES function.
If your LES is not working well, there are a number of things that you may be doing that promote reflux and cause you to experience heartburn.
Tips for Preventing Reflux
Your posture
Gravity plays an important role in controlling reflux. Lying down after a large meal can overwhelm a less than perfect LES. Food comes back into the esophagus and heartburn occurs.
If you experience heartburn, think whether it occurs after meals, when you lie in bed at night, or if you take a nap after a meal. Maintaining an upright posture until the meal is digested may prevent the heartburn.
If heartburn occurs regularly at night, consider raising the head of the bed or inserting a triangular wedge to keep your esophagus above the stomach.
Avoid physical exertion after a meal. It contracts the abdominal muscles and forces food through a weakened sphincter. This is especially true of tasks that require bending such as lifting or cleaning the floor.
How you eat
How is perhaps more important than what you eat. A large meal will empty slowly from the stomach and exert pressure on the LES. A snack at bedtime is well positioned to reflux when you lie down.
It is best to eat early in the evening so that the meal is digested by bedtime. You might try having the main meal at noon and a lighter one at dinnertime.
All meals should be eaten in relaxed stress-free surroundings. If possible, stay seated during, and for a time after, eating.
Smaller meals and an upright, relaxed posture should help minimize reflux.
What you eat
Certain foods compromise the sphincter’s ability to prevent reflux, and are best avoided before bedtime or exertion.
These differ from person to person, but many recognize these foods as particularly troublesome:
- Fats
- Onions
- Chocolate
Alcohol often provokes heartburn by compromising the LES, irritating the esophagus, and by stimulating stomach acid production.
Certain other foods may bother some people. When you notice a food provokes your heartburn, try avoiding or reducing it for a period of time.
Some oral medications will burn if allowed to rest in the esophagus. To be safe, always swallow medication in the upright position and wash it down with water.
Other factors
Being overweight can promote reflux. Excess abdominal fat puts pressure on the stomach and the loss of even a moderate amount of weight makes many people feel better.
Learn more about reducing heartburn by burning calories
Pregnant women are often troubled by heartburn, particularly in the first three months. Certain hormones appear to weaken the LES, and the increasingly crowded abdomen encourages reflux. Generally, if there has not been too much weight gain during the pregnancy, a woman’s heartburn improves after delivery.
Stress or strong emotion can also influence heartburn.
The most important measures are suggested by the information mentioned above. Avoidance of lying down or straining after meals, and elevation of the head of the bed are important.
Early dinners, smaller meals and the avoidance of fat, chocolate, and onions also seem particularly helpful. A review of diet, medications, and the stresses of life may help you manage the symptom.
When these measures fail an antacid preparation may temporarily relieve the symptom by neutralizing stomach acid. An antacid containing an alginate will float in the stomach and prevent reflux by blocking the lower esophagus. These are safe if used in moderation and as directed. There are now over-the-counter drugs that reduce acid production and may be safely taken for a few days until the heartburn subsides.
Complications
If the heartburn occurs on 2 or more days per week despite the measures discussed above, you should consult your family doctor.
If you are over 50 years old, your heartburn occurs with exercise, or you have a family history of heart disease, you should promptly see a physician to be sure that your heart is not the source of the pain.
See a doctor promptly if you experience difficulty swallowing, vomiting, passing blood, or significant weight loss.
If your heartburn is accompanied by breathing difficulties or hoarseness, you should seek medical advice.
Acid-Suppressing Drugs
There are powerful drugs that your doctor may prescribe for persistent symptoms, and tests may be done to exclude other diseases. The acid-suppressing action of these drugs controls the symptom of heartburn, but the conditions that cause reflux remain. Therefore, the heartburn is likely to return once the drugs are stopped.
Many people learn to control heartburn without using acid-suppressing drugs. The posture and eating modifications mentioned above remain an important part of treatment.
Nevertheless, persistent heartburn, or complicated GERD may require medication therapy to permit healing and prevent recurrence. This therapy should be done under the guidance of a physician.
Adapted from IFFGD Publication: Heartburn: Nothing to do with the Heart by W. Grant Thompson, MD, FRCPC, Emeritus Professor of Medicine, University of Ottawa, Ontario, Canada.









